The Gut-Brain Connection: How Your Microbiome Shapes Mental Health
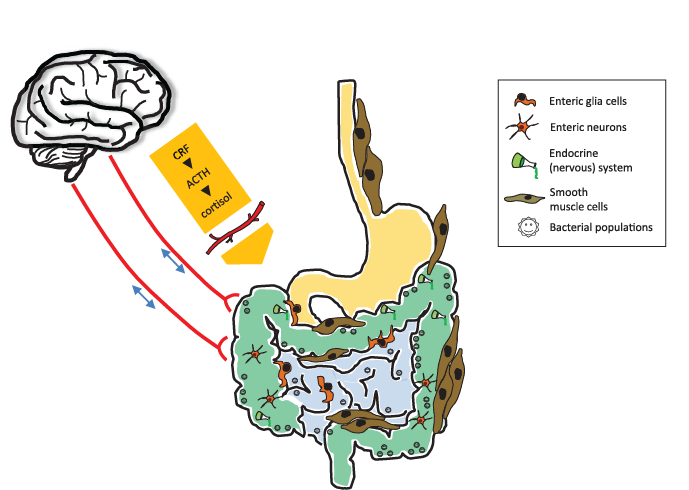
In recent years, scientists have begun to uncover a powerful relationship between the gut and the brain. This complex communication system is called the gut-brain axis. It involves constant two-way communication between your gastrointestinal (GI) tract and your central nervous system (CNS). While the brain is usually seen as the control center of the body, your gut microbiome the trillions of bacteria and other microbes living in your intestines plays a surprising and important role in shaping your mood, cognition, and mental health.

What Is the Gut Microbiome?
The gut microbiome refers to the community of microorganisms (mostly bacteria, but also viruses, fungi, and archaea) that live in your digestive tract, especially in the large intestine. Each person’s microbiome is unique, shaped by genetics, diet, lifestyle, and environmental exposure.
These microbes aren’t just passive passengers. They help digest food, produce vitamins like B12 and K, and protect against harmful pathogens. Most importantly for this discussion, they produce chemicals that affect brain function such as short-chain fatty acids (SCFAs), neurotransmitters, and immune molecules.
Gut Health and Mental Disorders
A growing number of studies show that changes in the gut microbiome are linked to several mental health conditions

Depression
People with depression often show reduced microbial diversity in their guts. Certain beneficial bacteria like Lactobacillus and Bifidobacterium are found in lower levels. These bacteria are known to produce GABA and serotonin, neurotransmitters that regulate mood.

Anxiety
Gut bacteria can influence the body's stress response by affecting cortisol levels and altering nervous system activity. In animal studies, germ-free mice (born without microbes) show increased anxiety-like behaviors, which can be reversed by restoring gut bacteria.

Autism Spectrum Disorder (ASD)
Children with autism often have different gut microbiome profiles and more frequent gastrointestinal issues. Some small clinical studies suggest that modifying the gut microbiome through diet or probiotic therapy can improve behavioral symptoms.

Cognitive Decline
There is growing interest in how gut health affects neurodegenerative diseases like Alzheimer’s. Inflammation originating in the gut may contribute to brain inflammation, potentially worsening memory and cognitive function.
How Microbes Talk to Your Brain
Your gut microbes can produce or influence levels of key brain chemicals, including
Dopamine: Some gut bacteria can stimulate dopamine production, which is linked to motivation and pleasure.
SCFAs (short-chain fatty acids): These are made when bacteria break down fiber. SCFAs help reduce inflammation and protect the blood-brain barrier.
GABA (gamma-aminobutyric acid): A calming neurotransmitter produced by bacteria like Lactobacillus rhamnosus.
Serotonin: About 90% of the body’s serotonin is produced in the gut. While most of this stays in the GI tract, it still plays an indirect role in mood regulation.
How to Support Your Gut for Better Mental Health
Eat More Fiber
Fiber-rich foods like fruits, vegetables, legumes, and whole grains feed your beneficial bacteria and promote the production of SCFAs.
Add Fermented Foods
Yogurt, kefir, sauerkraut, kimchi, and miso contain live probiotics that can help restore microbial balance.
Avoid Ultra-Processed Foods
Highly processed, sugary, and high-fat diets are associated with gut dysbiosis (an imbalance in the microbiome) and increased inflammation.

Consider Probiotics and Prebiotics
Some studies suggest that "psychobiotics" probiotics with mental health benefits may help with anxiety and depression. Common strains include Lactobacillus and Bifidobacterium.
Manage Stress
Chronic stress can damage the gut lining and negatively affect the microbiome. Activities like meditation, yoga, and physical exercise support gut-brain harmony.